Understanding How Long Lisinopril Takes to Work
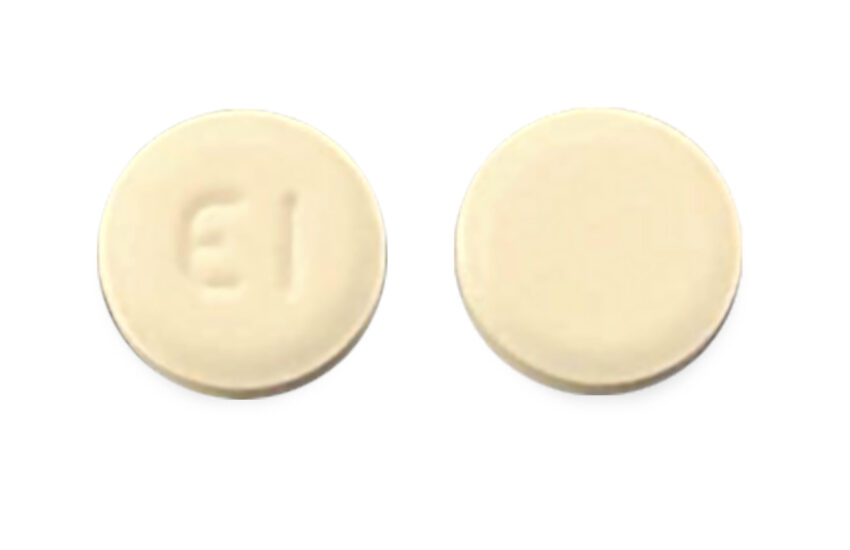
Lisinopril is a commonly prescribed medication for managing hypertension and heart failure. Patients often wonder about the how long lisinopril takes to work and its duration of action. This article provides in-depth insights into the various factors that influence its onset, effectiveness, and therapeutic timeline.
Lisinopril Onset of Action
The lisinopril onset of action typically begins within one hour after administration. However, the full therapeutic effect may take longer to be noticeable. The medication works by inhibiting the conversion of angiotensin I to angiotensin II, a crucial factor in blood pressure regulation. This mechanism in turn leads to lowered resistance in blood vessels, facilitating lower blood pressure levels. Most patients will notice a significant change in their blood pressure within the first 2 to 4 weeks of treatment. Understanding this time to effect is vital for patients expecting immediate results from their treatment.
Factors Affecting Lisinopril’s Onset
While the average onset of action for lisinopril is around one hour, individual factors can affect this timing. Age, weight, and existing healthcare conditions play roles in how effectively the medication acts. For instance, older adults may experience a slower response due to altered metabolism and organ function. Additionally, the presence of comorbidities such as diabetes or kidney impairment can influence how quickly lisinopril will start to lower blood pressure levels.
Patient Adherence and Its Impact
Compliance with the prescribed lisinopril dosage timing is essential for achieving meaningful results. Skipping doses or taking the medication inconsistently can lead to inconsistencies in therapeutic effects. Patients should incorporate lisinopril into their daily routine, ideally taking it at the same time each day to maintain stable medication levels in their bloodstream.
Lisinopril Duration of Action and Half-Life
The duration of action for lisinopril generally spans from 24 to 48 hours, making it a convenient once-daily medication. This extensive duration helps manage blood pressure throughout the day, contributing to its effectiveness in hypertension management. The half-life of lisinopril is approximately 12 hours, which allows for a sustained action within the body longer than some other antihypertensive medications.
Monitoring Therapeutic Effects
To optimize treatment, regular monitoring of lisinopril medication effects is necessary. Physicians often recommend routine blood pressure checks and blood tests to assess kidney function while on lisinopril. Full benefits are typically realized after a month of continuous therapy, but regular evaluation assists healthcare providers in adjusting lisinopril dosages or entirely changing medications if needed.
Comparative Analysis with Other Medications
Understanding how lisinopril compares to other antihypertensive medications can also illustrate its time to effect. For instance, diuretics usually have a quicker initial action, but the longer-term control of blood pressure is more favorable with lisinopril. It’s essential to discuss with healthcare providers about lisinopril interactions with other medications or therapies that patients are undergoing for concurrent health issues.
Lisinopril for Hypertension and Heart Failure
Lisinopril serves dual functions for treating both hypertension and heart failure, and its therapeutic effects manifest uniquely in each case. When used for hypertension, the goal is to lower blood pressure consistently, while in heart failure patients, lisinopril helps reduce strain on the heart muscle.
Understanding Lisinopril Effectiveness for Specific Populations
Studies indicate that the effectiveness of lisinopril may vary among populations, particularly in elderly patients or those with chronic kidney conditions. For elderly patients, doctors may begin with lower starting doses to evaluate individual tolerance and reaction before gradually adjusting according to the patient’s response. This personalized dose adjustment enhances safety and efficacy.
Lisinopril Side Effects and Monitoring
While lisinopril is an effective medication, patients should be aware of its potential side effects. The most common are dizziness, headaches, and potential changes in kidney function. Patients should be vigilant about monitoring these effects through blood tests. Awareness of lisinopril side effects onset can significantly aid in identifying complications early. If severe adverse reactions occur, contacting a healthcare provider is advised.
Practical Steps for Patients Using Lisinopril
Adopting practical steps while using lisinopril for hypertension can optimize treatment outcomes. This can include healthy lifestyle choices such as dietary modifications, regular exercise, and avoiding drug interactions.
Daily Routine Integration
Integrating lisinopril into daily routines can significantly bolster treatment adherence. Patients might find it helpful to set daily reminders on their phones to ensure they do not miss a dose. Pairing the medication with a specific daily activity, like brushing their teeth, can also be an effective technique.
Health Guidance for Long-term Use
Patients should consult their healthcare providers regularly during long-term lisinopril treatment. This continuous dialogue is crucial for addressing potential issues like tolerance or changing health needs. Checking in allows for timely adjustments and ensures optimal management of hypertension or heart failure symptoms.
Key Takeaways
- Lisinopril usually takes about one hour to start working, with a full effect visible in 2-4 weeks.
- The medication has a duration of 24-48 hours, making it suitable for once-daily dosing.
- Effective management of hypertension and heart failure requires regular monitoring of blood pressure and kidney function.
- Patients should adhere to prescribed dosages and integrate the medication consistently into their daily routines.
- Open communication with healthcare professionals is vital for optimizing lisinopril therapy.
FAQ
1. How does lisinopril affect heart function?
Lisinopril can improve heart function significantly in patients with heart failure. The medication works by decreasing the workload on the heart and improving blood flow, which in turn helps manage symptoms such as shortness of breath and fatigue.
2. What should I monitor while on lisinopril?
It’s important to monitor blood pressure regularly and to have blood tests to check kidney function and potassium levels. Patients should also watch for any potential side effects and report these to their healthcare providers promptly.
3. Can I take lisinopril with other medications?
Yes, but it is crucial to inform your doctor about all medications you are taking. Lisinopril can interact with diuretics, potassium supplements, and other blood pressure medications, which may require dosage adjustments.
4. Are there specific warnings for using lisinopril?
Patients with a history of angioedema, especially related to ACE inhibitors like lisinopril, should avoid this medication. Additionally, those who are pregnant or intend to become pregnant should discuss alternatives with their healthcare provider.
5. Can lifestyle changes enhance the effectiveness of lisinopril?
Absolutely! Lifestyle changes—such as maintaining a balanced diet, engaging in regular physical activity, and managing stress—can significantly enhance lisinopril’s effectiveness. These changes support overall heart health and assist in achieving better blood pressure control.
By understanding the dynamics of how long lisinopril takes to work, patients can better manage their expectations and enhance their treatment journey.