Effective Ways to Calculate Cardiac Output: Essential Methods for 2025
Understanding **cardiac output** and its calculation is crucial for effective cardiac care. In this article, we will delve into the definition of cardiac output, explore various **methods to estimate cardiac output**, and examine the factors affecting this important physiological parameter in health and disease. Whether you are a healthcare professional or a student in medicine, the information here will provide you with a detailed guide on how to accurately assess cardiac output in various situations.
Definition and Significance of Cardiac Output
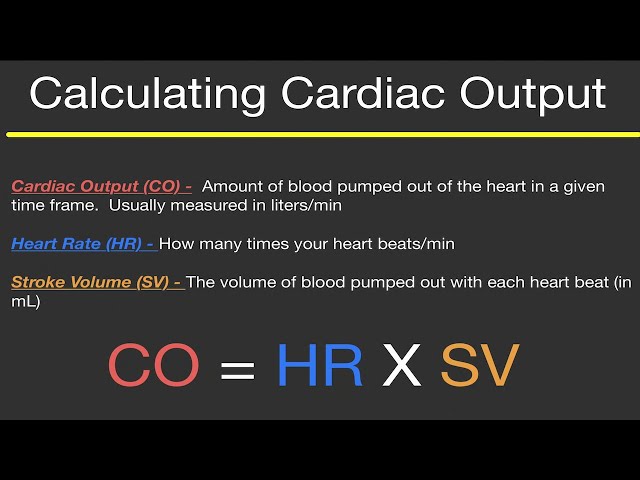
The term **cardiac output** refers to the amount of blood the heart pumps in a minute, representing a critical measure of heart’s pumping efficiency. It is calculated using the formula: Cardiac Output (CO) = Stroke Volume (SV) × Heart Rate (HR). A normal **cardiac output** ranges from 4 to 8 liters per minute, although this can vary based on activity and individual health status. Understanding the **significance of cardiac output** is integral because it provides insight into the heart’s functionality and patient’s fluid status, aiding in conditions like heart failure or during **exercise**. Besides its role in assessing cardiovascular health, it also serves as an essential indicator in **clinical settings**, guiding interventions and monitoring patient outcomes.
How Heart Rate and Stroke Volume Affect Cardiac Output
To comprehend **cardiac output** fully, it’s essential to analyze the two main components influencing it: **stroke volume** and **heart rate**. Stroke volume is the volume of blood pumped from the left ventricle with each contraction, which can be influenced by factors like blood volume, venous return, and muscular contraction strength. On the other hand,** heart rate**, the frequency of heartbeats per minute, directly impacts how much blood is circulated in the body. During periods of **exercise**, the heart rate increases, resulting in a higher cardiac output to meet increased metabolic demands. Conversely, in a resting state, a lower heart rate corresponds to a reduced cardiac output, emphasizing the balance necessary for healthy cardiovascular function.
Understanding Cardiac Output Units and Measurements
Typically, **cardiac output** is expressed in liters per minute (L/min). For clinical analysis, understanding the methods of **cardiac output measurement** is vital. Two primary techniques exist: **invasive and non-invasive cardiac output measurement**. Invasive methods involve inserting catheters, usually during surgery or in intensive care units, to gather precise data about cardiac function. In contrast, non-invasive methods rely on echocardiographic techniques to measure stroke volume and ultimately arrive at cardiac output values. Such techniques are essential in real-time monitoring and for understanding **cardiac performance** in **critical care** settings, reflecting immediate patient responses to treatments and interventions.
Methods to Estimate Cardiac Output
Various **methods to calculate cardiac output** have been developed over the years, each with its advantages and disadvantages. The choice of method depends on the clinical scenario, accuracy required, and patient condition. Understanding these methodologies is essential for healthcare providers to ensure accurate assessments of **cardiac output**.
Cardiac Output Formula and Mathematical Models
The most recognized **cardiac output formula** utilizes the relationship between stroke volume and heart rate. Mathematically, it can also be represented in a variety of forms, accounting for parameters like body surface area, leading to the development of the **cardiac index**, which normalizes cardiac output relative to the individual’s size. This adjustment facilitates the interpretation of **cardiac performance** across different populations, heightening the clinical significance of these calculations. These mathematical models are particularly useful in areas like cardiology, where precision in evaluating cardiac dynamics is paramount.
Advanced Techniques in Cardiac Output Monitoring
Recent advancements have led to the emergence of non-invasive tools employing **sensor technology in monitoring cardiac output**. These devices extract data by measuring parameters like the velocity of blood flow or changes in the diameter of blood vessels during hemodynamic assessment. An illustration of this would be shared by applying advanced echocardiography. Such innovations not only improve patient comfort but also significantly enhance the accuracy of cardiac output estimations over traditional invasive techniques, allowing for near-real-time analysis without the risks associated with invasive procedures.
Factors Affecting Cardiac Output: Clinical Implications
Identifying various factors that influence **cardiac output** is critical, particularly in a clinical context. A comprehensive understanding empowers healthcare professionals to assess heart function more effectively and make informed treatment decisions regarding conditions like **heart failure**.
The Impact of Body Position and Temperature on Cardiac Output
One notable factor is how **body position** can significantly alter **cardiac output** parameters. For example, when transitioning from lying down to sitting or standing, the gravitational shift can affect venous return and heart efficiency. Similarly, **temperature changes** also affect cardiac function, with hyperthermia often leading to elevated heart rates and resultant increases in **cardiac output**, which compensates for enhanced metabolic activity during heat stress. Recognizing these dynamics is particularly relevant in clinical assessments and during procedures where patient positioning may fluctuate.
Exercise Physiology: Dynamics and Role of Cardiac Output
During **exercise**, cardiac output undergoes remarkable changes. Increased activity demands lead to an upsurge in both heart rate and stroke volume, thereby amplifying **cardiac output** to ensure adequate oxygen supply to the muscles. This physiological adaptation showcases the body’s ability to maintain hemodynamic status amidst increased workloads. During peak performance days, like a rigorous athletic training session, these adjustments become even more crucial, de-emphasizing risk factors tied to **low cardiac output** conditions or heart-related complications.
Cardiac Output in Special Populations
Understanding the nuances of **cardiac output** is especially valuable when considering special populations, such as pediatric patients or those who are pregnant. Variability occurs due to differing bodily demands and heart functions in these groups.
Cardiac Output in Pregnancy
In pregnancy, a woman’s **cardiac output** can increase significantly by 30-50% as the body works to accommodate the increased metabolic needs of both the mother and developing fetus. This involves an elevation in both stroke volume and heart rate until the female’s body stabilizes around the third trimester. Recognizing these changes is vital for managing pregnancies, identifying any complications early, and ensuring healthy outcomes for both mother and baby, notably when overseeing pregnancy-related cardiac care.
Assessing Cardiac Output in Pediatrics
In pediatric populations, calculating **cardiac output** must carefully consider age and developmental stages, where normal values differ significantly from adults. Pediatricians employ tailored methods relating to **normal cardiac output** expectations during various growth phases, which underscores the importance of using appropriate reference values and assessing with comparative benchmarks suitable for children to avoid misinterpretation of heart function and possible health concerns. Achieving a nuanced understanding through regular assessments fosters effective monitoring of children’s health and development.
Key Takeaways
- **Cardiac output** is a essential indicator of heart health, influenced by factors like **stroke volume** and **heart rate**.
- Multiple methods can accurately assess cardiac output, including invasive and non-invasive techniques.
- Clinical consideration of variables, such as patient position and temperature, is necessary for accurate **cardiac output assessment**.
- Special populations, including pregnant individuals and children, have unique cardiac output dynamics that must be understood.
FAQ
1. What are the normal ranges for cardiac output?
Normal **cardiac output** ranges from 4 to 8 liters per minute in healthy adults. However, values can vary depending on factors like age, fitness level, and body size, requiring clinicians to adapt assessments contextually for accurate evaluations. Monitoring** cardiac output values in different populations** is vital for understanding individual cardiac health based on demographic factors.
2. How does exercise affect cardiac output?
During **exercise**, cardiac output typically increases as both stroke volume and heart rate rise to meet the physical demands of working muscles. This dynamic change allows the heart to deliver more oxygen-rich blood to the muscles, enabling sustained performance while managing metabolic waste effectively.
3. What are the implications of low cardiac output syndrome?
Low **cardiac output syndrome** indicates that the heart does not pump sufficiently to meet the body’s needs, often leading to poor organ perfusion and metabolic imbalance. This condition warrants prompt medical attention, as it can result from various diseases or acute episodes and requires a targeted treatment approach to improve cardiac performance.
4. Can **medications** affect cardiac output?
Yes, various **medications can impact cardiac output** by influencing heart rate, contractility, or afterload. Beta-blockers, for example, may decrease heart rate and, subsequently, cardiac output, while inotropes increase contractility and potentially improve output in heart failure scenarios.
5. How is cardiac output monitored in intensive care?
In an intensive care setting, **cardiac output monitoring** is often done through invasive methods, such as pulmonary artery catheterization, or non-invasive techniques like echocardiography. This enables real-time tracking and adjustment of therapies based on the patient’s hemodynamic status, which is essential for managing critically ill patients effectively.
6. What role does the autonomic nervous system play in cardiac output?
The **autonomic nervous system** regulates heart rate and contractility, significantly influencing **cardiac output**. During stress or physical exertion, sympathetic stimulation increases heart rate and contractility, thus enhancing cardiac output and ensuring sufficient blood flow to meet heightened metabolic demand.
7. How do cardiovascular diseases affect cardiac output?
**Cardiovascular diseases** often impair cardiac output by affecting the heart’s ability to contract or pump blood effectively—leading to conditions like heart failure, where reduced output can compromise organ function and overall health. Understanding how these diseases alter hemodynamics is crucial for effective management and patient outcomes.